Urgent stroke care
in England is still being impacted by Covid-19
Our viewpoint
3 August 2023
Strokes are responsible for approximately 38,000 deaths every year in the UK, and around two-thirds of an estimated 1.3 million stroke survivors suffer from disabilities that hinder their ability to live independently and require extensive healthcare treatment.
- Stroke patients need urgent medical care as soon as symptoms are noted if they are to have the best possible outcome.
- Ambulance waiting times are still too long for suspected stroke and other medical emergencies.
- Patients with stroke in England are taking longer to get to hospital and waiting longer for the key treatments and urgent specialist care they need.
- As a result of these delays, more patients may be left with long-term disability, profoundly impacting not only the lives of stroke patients, but also their families, and caregivers, as well as placing a significant burden on wider NHS resources.
Despite being beyond the acute phase of the Covid-19 pandemic, the ability of the NHS to deliver essential stroke-related care seems to remain compromised. Our latest research used public Sentinel Stroke National Audit Programme (SSNAP) and NHS ambulance data to assess the quality of care for acute stroke patients admitted to NHS hospitals.
Prolonged ambulance wait times in England are only part of the picture
In England, “Category 2” emergency responses, covering severe conditions like strokes and heart attacks, have a target time of 18 minutes. However, by December 2022, typical waiting times had reached 90 minutes, up from 20-30 minutes at the start of the pandemic in 2020. Despite some improvement in 2023, waits still average over 30 minutes, far exceeding the target (Figure 1).
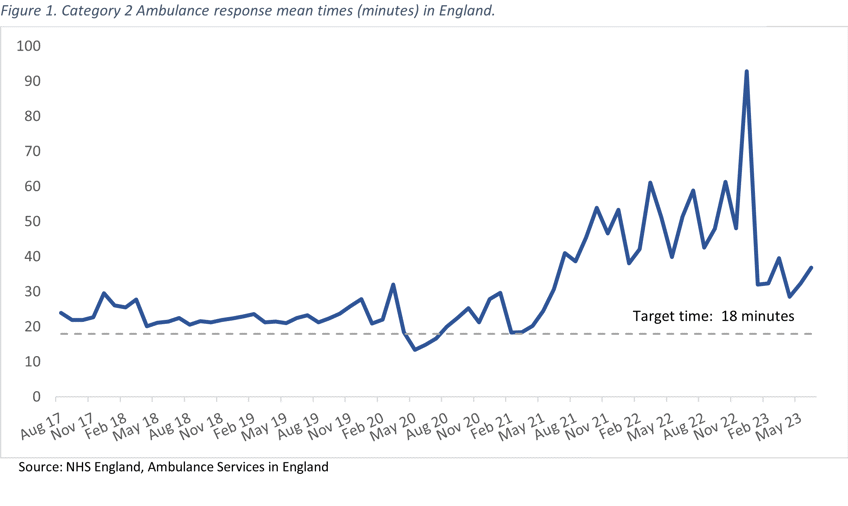
Figure 2: Stroke care pathway
But it’s not just about the time it takes for an ambulance to arrive. Patients with stroke symptoms need urgent medical care, which can prevent severe disability or even death. Moreover, a swift response could speed up the recovery process and open more treatment options, such as treatment with clot busting medicines (thrombolysis) or clot removal interventions (thrombectomy). These treatments need to be given quickly after stroke to be effective.
We analysed the NHS stroke care timeline, encompassing both pre-hospital and hospital services, for suspected stroke patients (Figure 2). Since March 2020, worrying trends have emerged.
Late arrival delays the start of treatment
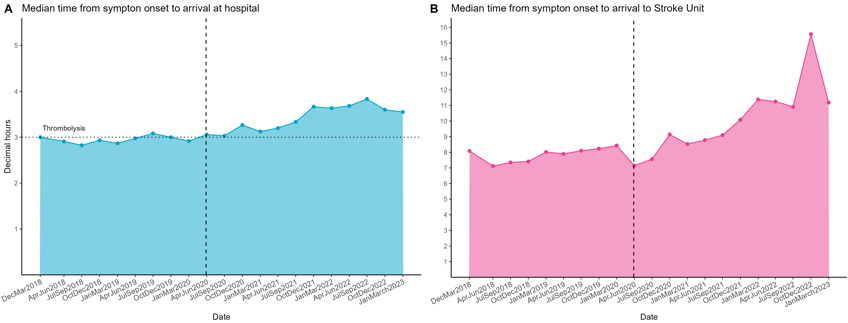
The median ambulance journey time, from the onset of symptoms to hospital arrival, has increased by an average of one hour and is now nearly four hours (Figure 3.A). This delay risks excluding stroke patients from treatments like thrombolysis, because they miss the three-hour window for it to be started. Furthermore, the later thrombolysis begins, the worse the prognosis, resulting in fewer patients achieving minimal or no disability three months after their stroke.
Delayed admission to a Stroke Unit impacts recovery
The median time for a stroke patient's admission to a Stroke Unit increased by eight hours between October 2019 and December 2022. Despite improvements during 2023, the median time a patient waits to be admitted in a Stroke Unit is currently over 11 hours, far exceeding the national target of within four hours of arrival (Figure 3.B). Admission to a Stroke Unit significantly improves patient outcomes and saves lives. Patients receiving organised in-patient care in these units are more likely to be alive, independent, and living at home one year after a stroke.
Figure 3: Median time from the onset of symptoms to achieve the key events of stroke care
Fewer patients are receiving the care they need when they need it
The quality of care that patients receive after arriving at hospital has deteriorated. Between October-December 2019 and October-December 2022, for every 100 people admitted to hospital with acute stroke, there were around 14 fewer patients admitted to a stroke unit within four hours of arrival. Approximately 1 in 10 of the patients who would have received thrombolysis in October-December 2019 are now not doing so, and the proportion of patients receiving thrombolysis within one hour has fallen (Table 1).
Patients have also been waiting longer for timely assessment by stroke specialists and the multidisciplinary team supporting patients in their recovery.
Table 1: Stroke care quality metrics
|
Quality metric |
Oct-Dec 2019 |
Oct-Dec 2022 |
|
First Ward |
||
|
Stroke Unit |
80.3% (18,304) |
77.3% (17,587) |
|
MAU/AAU/CDU |
11.4% (2,605) |
12.0% (2,723) |
|
ITU/CCU/HDU |
2.6% (603) |
3.0% (682) |
|
Other |
5.6% (1,282) |
7.8% (1,774) |
|
Intravenous Thrombolysis (Ischaemic only) |
11.5% (2,617) |
10.4% (2,360) |
|
Intravenous Thrombolysis within 1h (if thrombolysed) |
61.8% (1,618) |
58.7% (1,385) |
|
Mechanical Thrombectomy (ischemic only) |
1.6% (357)* |
3.3% (752) |
|
Brain scan within 1h |
55.3% (12,613) |
56.6% (12,895) |
|
Swallow screen within 4h (if applicable) |
68.3% (15,577) |
66.6% (15,163) |
|
Direct admission to Stroke Unit within 4h (if applicable) |
53.3% (11,653) |
39.5% (8,515) |
|
Stroke specialist nurse assessment within 24h |
91.3% (20,816) |
89.1% (20,288) |
|
Stroke specialist physician assessment within 24h |
84.1% (19,167) |
83.3% (18,954) |
|
Stroke specialist assessment within 72h |
95% (21,665) |
94.1% (21,418) |
|
Method of stroke assessment |
||
|
In person |
77.2% (17,607) |
74.9% (17,063) |
|
Telemedicine (video) |
3.2% (721) |
5.8% (1,318) |
|
Phone |
15.7% (3,576) |
14.8% (3,363) |
|
No First Contact |
3.9% (890) |
4.5% (1,022) |
|
Physiotherapy assessment within 72h (if applicable) |
95.3% (19,227) |
92.5% (18,598) |
|
Not eligible for physiotherapy |
11.5% (2,621) |
11.7% (2,670) |
|
Occupational therapy assessment within 72h (if eligible) |
92.7% (18,427) |
89.0% (17,555) |
|
Not eligible for occupational therapy assessment |
12.8% (2,924) |
13.4% (3,045) |
|
Swallow assessment within 72h (if eligible) |
89.1% (7,366) |
86.1% (7,849) |
|
Not eligible for swallow assessment within 72h |
63.7% (14,526) |
59.9% (13,645) |
|
Communication assessment within 72h (if eligible) |
90.2% (10,734) |
86.3% (10,643) |
|
Not eligible for communication assessment |
47.8% (10,897) |
45.8% (10,434) |
|
90% stay in stroke unit (if applicable) |
83.1% (18,263) |
73.3% (15,664) |
* Note: Data is from July to Sept 2019 as it was unavailable during the period of Oct 2019 to Dec 2019
Is there an increase in younger patients having stroke?
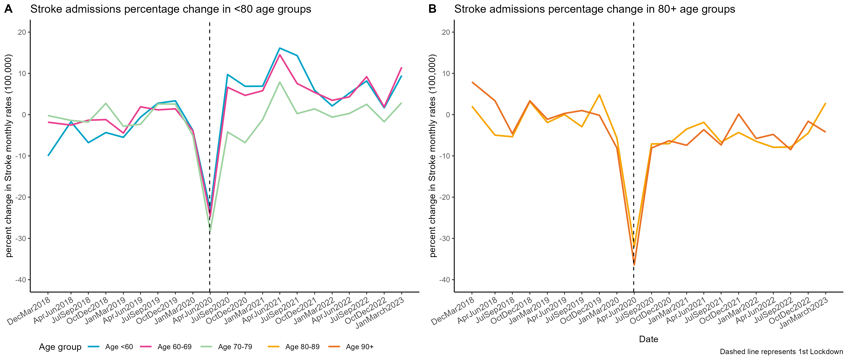
Our analysis also suggests that the Covid-19 pandemic has had differential impacts on stroke patients based on their age. We analysed the change in stroke admission rates per age group against the mean rate of all stroke admissions for 2019. Our findings revealed a substantial decrease (~30%) in admissions for all patients during the pandemic's initial phase, with trends varying according to patient age thereafter.
We observed an increase (~10%) in stroke admissions for those under 70 years old (including both those under 60 and those aged 60-69) after the pandemic first hit. While these trends warrant further investigation, they may hint at shifts in cardiovascular risk factors, such as a potential association between Covid-19 infection and stroke, or disruptions in the prevention and management of stroke-prone conditions like atrial fibrillation and hypertension.
In contrast, there has been a steady decline (~7%) in admissions among elderly patients (those aged between 80-89 and 90+ years). The "healthy survivor bias" could be a contributing factor - as there were such larger numbers of excess deaths in those age groups in the first year of the pandemic, that displacement of death from those who might have been expected to die in subsequent years may mean the resulting older population is on aggregate more healthy and has a lower risk of several acute events, such as stroke, than had the pandemic not occurred.
Figure 4: Stroke admission rates percentage change per age group in England 2017-2022
Far-reaching consequences
The big improvements in acute stroke care quality that the NHS has delivered over the past decade appear to have been undone to some extent in the aftermath of the Covid-19 pandemic and appear to be continuing to deteriorate in several aspects.
If a significant number of patients have been deprived of timely interventions like thrombolysis or prompt stroke unit admission, it is likely that more patients will have poor outcomes after stroke, such as death or long-term disability.
Getting stroke care back on track should be a priority for the NHS if these far-reaching consequences, that include not only the patient but their family and caregivers, and the wider society, are to be avoided.

